Gastric Outlet Obstruction – Symptoms, Treatment, Surgery
What is Gastric Outlet Obstruction?
Gastric outlet obstruction is a disorder wherein there is an obstruction in the opening of the stomach (Pylorus), blocking the entrance of ingested food coming from the stomach to the duodenum.
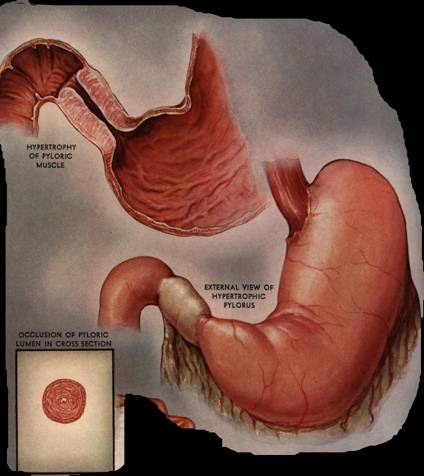
Gastric outlet obstruction showing Pyloric stenosis
Gastric Outlet Obstruction Symptoms
- Vomiting – Vomiting is a characteristic clinical symptoms. Usually right after eating, output is either yellow or green. It also contains foods eaten more than 12 hours earlier.
- Epigastric pain – Usually felt in the upper part of the abdomen, accompanied by acute pain that worsens.
- Constipation – Passing of stool is difficult and painful due to dry and hardened feces.
- Loss of weight – Sudden weight loss occurs due to fluid loss and poor appetite.
- Hypokalemia and metabolic acidosis – Due to vomiting, there is a loss of electrolytes like potassium and may lead to metabolic acidosis.
- Satiety
- Feeling of heaviness especially after meal
- Difficulty and painful swallowing of food
- Abnormal enlargement of the stomach – Hypertrophy of the muscles in the stomach may be present because of obstruction.
Gastric Outlet Obstruction Causes
Peptic ulcer disease
PUD is the most common cause of Gastric outlet obstruction, approximately 60% to 65% of total cases. The obstruction often occurs in the duodenum, and sometimes in the pyloric channel, prepyloric gastric antrum, and in rare cases, in the body of the stomach. Peptic ulcer disease is followed by narrowing of the lumen and the outcome is sudden contraction of the stomach muscles, inflammation and edema.
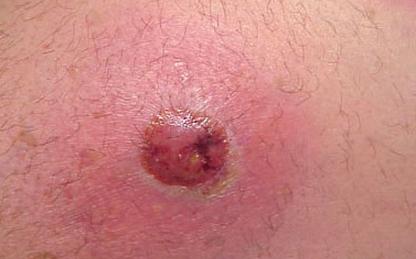
Malignant Tumor
The second most common cause of gastric outlet obstruction, for about 30% to 35% of all cases. Lesions usually appear near the pylorus, symbolizing carcinoma of the antrum and it grows circumferentially.
Benign Tumor
In rare cases, benign polyps in the pylorus can cause gastric outlet obstruction. The polyps are pushed into the duodenum through peristalsis.
Inflammatory diseases
Inflammatory disorders can cause accumulation of excess amount of fluids and sudden muscle contraction that may lead to gastric outlet obstruction. Crohn’s disease commonly develops obstruction. Others are Sarcoidosis, Tubercolosis and Syphilis has been reported to be contributing factor in thickening of the gastric wall that may lead to obstruction. Pancreatitis and cholecystitis can stimulate inflammatory contractions that may result in the destruction of proximal duodenum lumen and gastric outlet obstruction.
Organoaxial volvulus
Twisting of the stomach on itself is also one cause of gastric outlet obstruction.
Ingestion of Foreign Body
This happens very uncommonly. Unintentional among many, but in patients who are mentally impaired, they commit it intentionally.
Diagnosis
Physical Assessment
Physicians initially perform physical examinations on the suspected patients. Auscultation and percussion of the stomach are done by the physician as part of the assessment. There can be a palpable lump in the epigastric region or a splashing sound can be heard in a dilated stomach.
Barium Meal
Ingestion of barium sulfate followed by x-rays to visualize the stomach and duodenum. It reveals positive abdominal distention and narrowing of the pyloric canal.
Endoscopy
It is a noniinvasive procedure that allows inner visualization of the upper gastrointestinal tract. The esophagus, stomach and duodenum are the involved. This procedure is used to detect gastric tumors and ulcers. Gastric juices can be also collected to be examined for malignant cells.
Abdominal ultrasound
The shadow image on the ultrasound displays distension and enlargement of the stomach.
CT Scan with contrast
Imaging through computed tomography with contrast displays tumors and obstructions in the stomach.
Electrolytes
Monitoring of electrolyte levels such as Potassium, Sodium, and Chloride. Imbalances in these electrolytes may occur due to continuous vomiting and dehydration.
Treatment
1. Proton pump inhibitors
These drugs are used to treat peptic ulcers. They decrease the secretion of gastric acid.
2. Nasogastric suction
A procedure wherein the gastric contents inside the stomach are drained. Using a plastic tube inserted in the nose to the small intestine to remove secretions. However, it is contraindicated among those with esophageal obstruction and blocked airway.
3. Electrolytes replacement
Electrolyte replacement is done to replace what is lost and to maintain the normal level and prevent complications.
4. Antrectomy
Surgical removal of the Antrum, part of the stomach just inside the pylorus.
5. Vagotomy
A surgical procedure that involves cutting one or more branches of the Vagus nerve. The Vagus nerve has a major role in producing and regulating gastric acid secretions. It typically reduces the rate of gastric secretion, usually used in treatment of a peptic ulcer.
6. Billroth I
It is the removal of the Pylorus and the proximal stomach is connected to the duodenum. For the treatment of peptic ulcer and gastric cancer
7. Gastrojejunostomy
Also called Billroth II, it is a surgical procedure that creates a connection between the jejunum (the middle part of the small intestine between the duodenum and ileum) and the stomach. This allow gastric contents to directly enter the jejunum and for proper food absorption.
8. Parenteral Nutrition
Supplementary nutrients via Total Parenteral Nutrition (TPN) or Distal feeding tube are beneficial among patients with gastric outlet obstruction since their nutritional status gets worse.