Maple Syrup Urine Disease – Pictures, Symptoms, Treatment, Diagnosis
What is Maple Syrup Urine Disease (MSUD)?
Maple Syrup Urine disease is a congenital condition characterized by a metabolic error involving branched-chain amino acids. The metabolic error results in urine with a distinctive sweet smell. It is also an autosomal recessive disease, which means the condition can be inherited.
What Happens When an Infant has Maple Syrup Urine Disease (MSUD)?
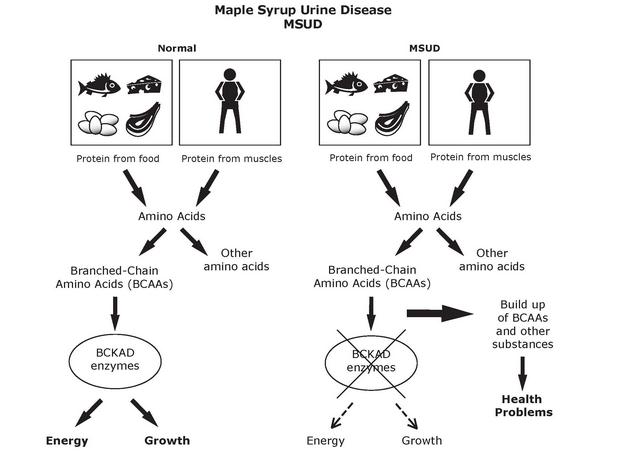
MSUD is a condition characterized by a faulty metabolism of branched-chain amino acids. Amino acids are the building blocks of proteins; proteins in turn are the building blocks of almost everything in the human body. Proteins are important components of muscles and bones, skin and internal organs, connective tissues, blood components and much more. Without amino acids, protein build up wouldn’t be possible, and without protein, building essential components of life also wouldn’t be possible.
There are three examples of branched chain amino acids: isoleucine, leucine, and valine. These amino acids are considered essential amino acids. They are called “essential” because they are not produced by the body (therefore we must get them from outside sources, e.g. diet) and are important in the regulation of certain body processes.
What happens with Maple Syrup Urine Disease is the body has defective enzymes to break down or catabolyze the branched chain amino acids. Breakdown or catabolism of these amino acids is an essential process so that the body can use the amino acids and also prevent them from accumulating in the body. Because the enzyme responsible for the breakdown is defective (as it cannot breakdown or process the amino acids properly), the amino acids accumulate. The accumulation of the amino acids poses a danger to the brain and overall neural function of the infant as these proteins and their byproducts are toxic. The condition can then lead to progressive degeneration of brain functions, seizures, coma and death, especially when left untreated.
What Causes Maple Syrup Urine Disease
Alterations in genes or gene mutations are said to be the primary cause of Maple Syrup Urine Disease. Changes in the genes DBT, DLT, BCKDHA and BCKDHB cause the condition. These genes are responsible for instructing the cells to effectively process and break down the amino acids isoleucine, leucine, and valine. Because the genes are defective, proper instructions are not given to the cells, leading to a faulty processing of the proteins.
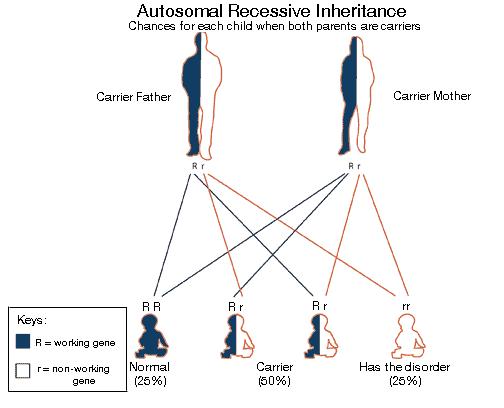
The gene mutations are inherited conditions and the disease follows an autosomal recessive pattern. This means each cell has both copies of the faulty gene. Parents of a person with an autosomal recessive disease carry a copy of the faulty gene, but most often the parents don’t manifest the signs and symptoms of the disease.
Symptoms of Maple Syrup Urine Disease
Maple Syrup Urine Disease (MUSD) symptoms depend on the extent or the type of MUSD they have. The signs and symptoms of MUSD according to its classification are listed below.
Classic Maple Syrup Urine Disease
Classic Maple Syrup Urine Disease is the most common and most severe type. The condition is present immediately or after 4 to 7 days from birth; symptoms of Classic MUSD are as follows:
- Vomiting
- Poor feeding
- Delay in breast feeding
- Problems in weight gain
- Progressive lethargy
- Muscular hypotonia and hypertonia (alternating)
- Dystonia
- Encephalopathy
- Seizures
- Pancreatitis
Intermediate Maple Syrup Urine Disease
This is a rare type of MUSD where symptoms can present themselves at any age. Signs and symptoms of this type of MUSD include:
- Delay in the development
- Neurological impairment
- Presence of seizures
Intermittent Maple Syrup Urine Disease
This ranks as the second most common type of MUSD. In this type children develop normally both physically and mentally, however signs and symptoms of MUSD appear when the patients experience catabolic stress and intercurrent conditions such as otitis media. Signs and symptoms of this type include:
- Lethargy
- Ataxia
- Coma
- Seizures
Thiamine Responsive Maple Syrup Urine Disease
Is another rare type of MUSD where patients respond to thiamine. Neurological signs and symptoms such as lethargy, seizures, ataxia, are present.
E3-deficient MSUD
This type is a very rare form of Maple Syrup Urine Disease. The signs and symptoms are almost similar to “intermediate” except that this type is accompanied by lactic acidosis. Other deficiencies of the disease include:
- Pyruvate
- BCKD
- Alpha ketoglutarate dehydrogenase complex
How Is Maple Syrup Urine Disease Diagnosed?
Maple Syrup Urine Disease can be diagnosed through the following:
1. Examination of clinical features
Physicians examine the infant or the child for neurological problems, and other signs and symptoms reflective of MUSD. The classic sign of MUSD is the sweet scent of urine.
2. Blood Enzyme Tests
Enzymes present in the blood are also tested to diagnose MUSD. Decreased levels of the enzyme BCKAD and an increase in BCAA are usually suggestive of the condition.
3. Molecular Gene Testing
This diagnostic test aims to identify the three genes associated with Maple Syrup Urine Disease; these genes are BCKDHA, BCKDHB and DBT.
How Is Maple Syrup Urine (MUSD) Treated?
Treatment for MUSD usually involves:
1. Dietary Restrictions
Once diagnosed, strict and permanent dietary restrictions are implemented. Patients must avoid food sources high in leucine and other branched chain amino acids. This can be done by calculating the individual’s tolerance to leucine and choosing food sources that are appropriate to the patient’s tolerance. This is done for the first 6-12 months of life. Strict monitoring and implementation of the diet is the mainstay treatment for MUSD.
2. Glucose Infusions and Insulin
Glucose infusions are done to manage metabolic decomposition. Insulin is also given to manage or promote anabolism.
3. Liver Transplants
This treatment is done on patients with the classic form of MUSD. A liver transplant may halt the progressive decline in neurological function patients have, but the procedure does not reverse the existing damage patients have suffered.
Pictures





 A child with Beckwith-Wiedemann Syndrome
A child with Beckwith-Wiedemann Syndrome

