Estrogen Side Effects, Uses, Advantages
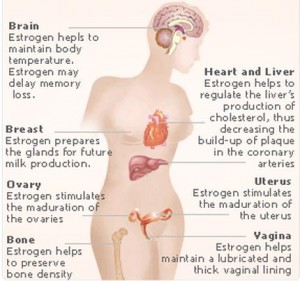
Estrogen is a group of sex hormones that is used by the body for various processes involving sexual, reproductive and metabolic functions. Estrogen is naturally occurring in the body, but it can also occur as an exogenous drug used for various conditions. It is naturally produced by the ovaries from cholesterol.
Estrogen occurs in the body as estradiol, estrone and estriol. Estradiol is the most predominant estrogen in the body. On the other hand, the other two estrogens are more predominant during pregnancy. Among the three, estrone is the most potent estrogenic substance while estriol is the least potent. Exogenous estrogen is available in various preparations such as:
- Chlorotrianisene
- Conjugated estrogens
- Dienestrol
- Esterified Estrogens
- Diethylstilbestrol
- Estropipate
- Ethinyl estradiol
- Quinestrolo
Uses and Advantages of Estrogen
Estrogen is used for various conditions. General indications of estrogen include:
- Treatment of hypoestrogenism
- Hormonal contraception
- Estrogen replacement therapy in menopausal women and those who have undergone oophorectomy or removal of the ovaries
- Infertility
- Management of prostate cancer
- Relief of symptoms of breast cancer
- Female hormone maintenance in male-to female transsexuals
Estrogen Side effects
Estrogen plays an important role in various process of the body such as the bones, liver, gene expression, blood clotting, and reproductive functions. The intake of exogenous estrogen may lead to various estrogen side effects related to its oral function. The various estrogen side effects include:
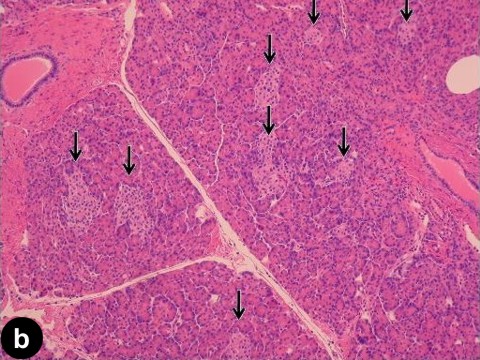
1. Ovarian, Endometrial and Breast Cancer
Estrogen use is also associated with the occurrence of various reproductive cancers as estrogen side effects. This occurs mainly as a result of binding to estrogen receptors that stimulate gene expression, which may damage the DNA and cause cellular proliferation resulting in malignancies.
2. Increase in uterine myomas
The presence of leiomyomas may be increased as estrogen side effect or aggravated by estrogen use because the development of abnormal, benign growths in the uterus is largely dependent on the presence of estrogen.
3. Increased blood clotting
Estrogen also is responsible for the production and utilization of the protein used for blood clotting. Prolonged use of estrogen contributes to the presence of abnormal blood clots leading to thrombophlebitis, deep vein thrombosis, and other clotting disorders that may potentially cause hypertension, stroke, heart attack and pulmonary embolism as estrogen side-effects.
4. Liver diseases
Estrogen use is also linked to the presence of cholestasis or the stasis if bile, which may eventually lead to advanced liver damage as estrogen side effect.
5. Fibrocystic breast changes
Transsexuals and men taking estrogen as hormone replacement or maintenance may have increased size of the breast as estrogen side effect
6. Changes in libido
Those taking estrogen therapies may also suffer from libido changes such as increase or decrease in libido as estrogen side effects. Being a hormone responsible for sexual functioning, initial intake of estrogen may reduce libido because the body is not used to the exogenous estrogen.
7. Nausea and vomiting
Nausea and vomiting are common estrogen side effects. These may occur especially at the start of the therapy and may eventually subside as the body gets used to the exogenous estrogen.
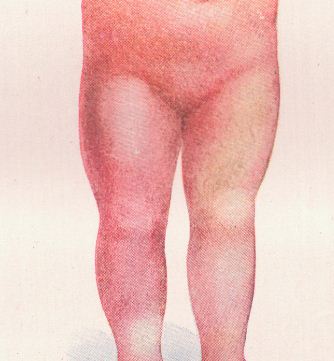
8. Weight changes
Estrogen may also cause weight changes as a result of water retention. People taking estrogen may experience weight gaining as an estrogen side effect.
Aside from the above common estrogen side effects, patients taking estrogen may also experience other estrogen side effects such as dysmenorrhea, scant menstruation, vaginitis, bloating and abdominal cramps, dyspepsia, diarrhea, Erythema multiforme, melasma or chloasma, pruritus, rash, retinal vascular thrombosis, Intolerance to contact lenses, dizziness, migraine, leg cramps, mood disturbances, and hemorrhoids.
In order to prevent these estrogen side effects and other side effects such as Nioxine side effects, proper and prudent use of medications should be employed. In addition, those who have increased risk for the above conditions should not consider taking estrogen. However, when estrogen use is needed, it is important to monitor the estrogen side effects and report them immediately to your health care provider.