Top 10 Vancomycin Side Effects
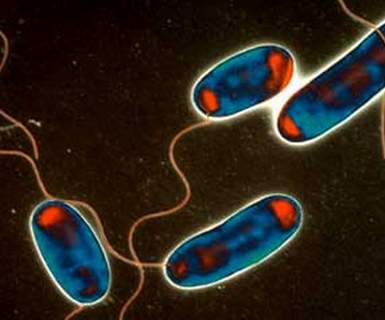
Unlike Rhodiola side effects, Co Codamol side effects or Flu jab side effects, Vancomycin is a pharmacological drug that is classified under glycopeptides antibiotic, which is famously used in the prophylaxis as well as the treatments that are brought about by gram positive bacteria. This is either to be used through the form of an oral route or an intravenous route. In addition to that, it is known to work to kill the bacteria and prevents its further growth. It will not work well with infections brought about by viruses.
The following are some of the benefits or advantages that one can get out of taking Vancomycin:
- Treatment from heart valve diseases
- Preventing endocarditis
- Treating infection in the intestines that causes colitis
The most important thing to consider when taking Vancomycin is that you follow the prescription of the physician. Only stop taking the drug for one week to be able to completely destroy and prevent the bacterial growth. Never take too much of what is recommended.
Vancomycin Side Effects
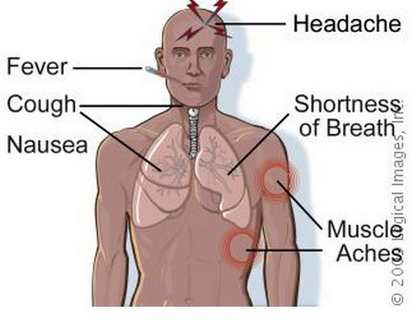
Despite the advantages that Vancomycin offers, there are also side effects to consider and to know prior to taking in Vancomycin. The following are some of the Vancomycin side effects:
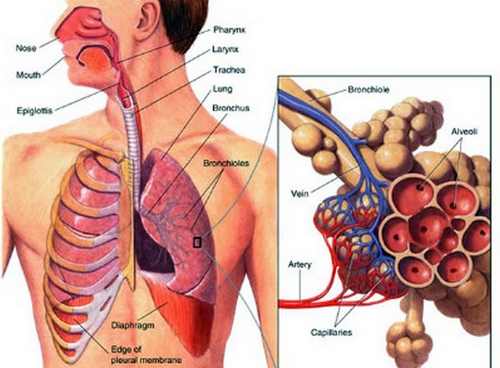
1. SORENESS OF THE THROAT
This is a common Vancomycin side effect. This happens because, despite the fact that the Vancomycin is designed to kill the harmful bacteria, it also has the tendency to kill both the positive and good bacteria, which are a big problem associated with its usage. This will then lead to the experience of soreness of the throat, which is a normal immune system response of the body when it is under attacked by foreign invaders.
2. TINNITUS
Tinnitus is a medical condition that deals with the ringing of the ears. Mild forms of tinnitus, part of the Vancomycin side effects, is another problem that imposes on persons taking in Vancomycin. The good thing about it is that it is a short lived side effect. Yet, it can lead to troublesome issues long term, which eventually leads to lifelong problems.
3. ITCHING THAT IS PERSISTENT
Another part of the Vancomycin side effects is itching that occurs persistently. This will usually manifest at long term use of the Vancomycin medication, and when it does start, it will lead to a long-lasting episode of itching.
4. BLURRING OF VISION
One of the Vancomycin side effects also includes blurring of vision which is transitory but the damage is permanent. Hence, there is a need to educate the person of this kind of side effect associated with the usage of Vancomycin.
5. CHILLS WHICH HAPPENS IN A PERIOD OF TIME
Chills are another thing to consider when you are taking in Vancomycin. Chills are included in the Vancomycin side effects, which exist not only because of the immune system response, but the fact that Vancomycin has a tendency to disrupt the chemical reaction of the body, which plays a vital role in the regulation of the body temperature.
6. UNUSUAL BLEEDING ISSUES
Another part of the Vancomycin side effects is having an unusual bleeding episode which affects the regulation of the blood flow. Vancomycin disrupts the clotting factor of a person, which may lead to unusualties in bleeding episodes.
7. ALLERGIC REACTION
This kind of Vancomycin side effect occurs rarely today. However, if such a reaction happens, you must report it immediately to your health care practitioner. The following associated symptoms under allergic reaction are: having difficulty breathing, rashes, swelling of throat or face or tongue, severe dizziness and itching episodes.
8. STOMACH PROBLEMS
This kind of Vancomycin side effect occurs especially when Vancomycin is taken via the oral route. Under this situation, the person taking Vancomycin might experience vomiting, nausea, indigestion, and stomachaches.
9. REDUCTION OF WHITE BLOOD CELLS
This is a rare Vancomycin side effect. However, when this happens, the person will be more at risk or prone to acquiring infections and much susceptible to the disease.
10. DAMAGE IN THE KIDNEY
Normally the Vancomycin, when taken orally or intravenously, is eliminated in the kidney. It can become toxic when high doses or prolonged therapy is given especially to the elderly with regards to the Vancomycin pharmacological treatment therapy. Hence, monitoring of the function of the kidney is of utmost importance when taking in this kind of medication.