Overactive Bladder – Symptoms, Medications, Treatment, Causes
What is an Overactive Bladder?
When urinary urgency happens even without the presence of urinary incontinent, the condition is called overactive bladder. This usually happens frequently or at night (Nocturia). Overactive bladder is more appropriately described as symptom syndrome, it is usually a symptom of an underlying condition rather that a separate disease itself. And it is a syndrome, in a sense that the condition is a combination of different symptoms.
Overactive Bladder: Who are the ones most affected?
This is a common condition that affects over 17% of women and men older than 40 years old.
Overactive Bladder Signs and Symptoms
You might have an overactive bladder if you experience the following symptoms:
Urinary urgency
This is a cardinal symptom of overactive bladder. Urinary urgency is defined as the sudden, strong urge to urinate that is hard to defer.
Urinary frequency
This is another symptom of overactive bladder. Urinary frequency is defined as urination of more than eight times a day.
Nocturia
Nocturia is defined as urination at night, prompting the individual to wake up more than once just to urinate.
Urge Incontinence
- This is the involuntary passage of urine (for no external reason) while having the feeling or urge to urinate.
- Overactive Bladder and its Impacts
- One’s quality of life is most affected by this condition; daily living and the different domains in life are significantly affected by an overactive bladder. These includes the following impacts
Self-esteem
This is the first domain usually affected by an overactive bladder. People with this condition become shy, feel guilty and fearful. They often perceive themselves as a burden to their friends and family. For this they may prevent themselves from social gatherings and interactions.
Socialization
The social aspect of a person with an overactive bladder is also greatly affected. Patients fear of losing control during social gatherings, and also of the odor of the urine when involuntary passage happens. Travel plans become limited only to area with nearby bathrroms.
Physical activity
Having this condition can limit one’s physical activity. Individuals may not be able to perform certain tasks or complete them because of the condition
Sexual function
Intimate relationships can also be affected by an overactive bladder. Patients with overactive bladder avoid sexual contact and intimate activities due to the fear of passing out and the odor of the urine.
Overactive Bladder Causes
The exact mechanism why overactive bladder happens remains to be elusive from experts and medical science. However, several theories have been proposed on the causes of an overactive bladder. These theories are the following:
The Myogenic Theory
The myogenic theory proposes that an overactive bladder happens as a result of partial loss of nerves in the bladder. This may be due to the following:
- Outlet obstruction in the bladder
- Increased pressure within the urinary bladder
This then leads to the alteration of the smooth muscles in the bladder, causing them to be more excitable. The increase in the bladder’s smooth muscle excitability causes micromotions of the detrusor muscle, this increase bladder pressure pushing urine out of the body.
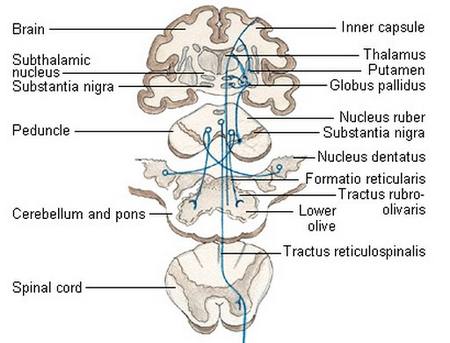
Suprapontine Inhibition
The suprapontine area is proposed to exert an action on the voluntary control of urination. MRI studies done on the suprapontine area indicate it has a participation in the control of urination, and individuals with damages on this area are seen to have voiding problems.
Acetylcholine from Urothelium
More recently, urothelium is discovered to be a factor in the development of an overactive bladder. The urothelium is a layer of epithelial tissue in the bladder and it may release greater amounts of acetylcholine. The increase in acetylcholine then triggers the activity of the brain and spinal cord, thereby giving the feeling of urinary urgency.
Other theorized causes of overactive bladder include:
- Damaged spinal cord and axonal pathways
- Loss of inhibition in the peripheries
- Increased afferent input in the lower urinary tract
- Cerebrovascular accident (stroke)
- Spinal Cord Injury (SCI)
- Multiple Sclerosis
- Neuropathies (diabetic neuropathy most commonly)
- Lesions in the brain especially on the suprapontine areas
Overactive Bladder Treatment
Overactive bladder therapy is treated with multiple approaches, but the first line treatment includes pharmacologic and behavioral therapy.
Pharmacologic Approach
Antimuscarinic agents
Pharmacologic therapy still remains to be the mainstay treatment of overactive bladder. The actions of antimuscarinic agents are:
- Inhibits acetylcholine from binding to the muscarinic receptors in the bladder preventing the reaction of bladder emptying (which leads to urination and a better bladder capacity.
- Inhibit sensory signals in the urothelium, decreasing signals to the brain and causing the brain to inhibit the voiding.
Five receptors are found all over the body, two of them are situated in the bladder, M2 and M3.
Currently and FDA approved antimuscarinic agents are as follows:
- Ditropan (oxybutin extended release)
- Detrol ( tolterodine tartate extended release)
- Oxytrol (transdermal oxybutin)
- Sanctura IR (trospium chloride immediate release)
- Vesicare (Solifenacin)
- Enablex (Daifenacin)
- Toviaz (fesoterodine)
- Gelnique (oxybutin chloride gel 10%)
Behavioral therapy
This is also employed but is seen most effective when done in conjunction with pharmacologic therapies. Behavioral therapy includes:
- Education on normal urination habits and normal bladder function
- Setting intervals even if the urge to urinate is not present
- Avoidance of caffeine, acidic and spicy foods which may exacerbate the symptoms
- Ample fluid intake- not too much or too little so the bladder would not be irritated
Overactive Bladder in Children
Overactive bladder can also occur in children but it is more physiologic than pathologic. For most cases, children are able to overcome an overactive bladder, certain studies have shown that almost 15% of the condition ceases after the age of 5.
Cause in Children
Among children, this can be a condition resulting from the immaturity of the nervous system. A child’s body still needs time to adjust or respond to the signals that regulate its function, and that includes urination.
Treatment in Children
When the child is unable to overcome the condition, medications and bladder training usually follows. Other techniques to manage this may also include the following:
- Caffeine free diet
- Scheduling the time of urination even without the urge to do so
- Learning how to relax the muscles during urination
- Teaching the child to how to urinate properly, nut rushing and taking time to urinate
Overactive Bladder in men
Men are also equally affected by this condition. This usually happens to men above the age of 40. Overactive bladder can have a myriad of causes that are only particular to men. These may include:
- Diverticulitis in the Bladder
- Stones in the Bladder
- Urinary Tract Infection
Treatment in Men
Overactive bladder can also be treated with a combination of medications and behavioral therapy.
Recent studies suggest that pelvic floor exercises can also be beneficial to men. pelvic floor exercises strengthens the muscles in the pelvis allowing the individual to gain more control on voiding. Pelvic floor exercises are usually done by females but recent studies reveal it is also beneficial to males as well.
Overactive Bladder Complications
Complications of overactive bladder include:
Ascending Urinary tract infections
This can result from prolonged exposure from the leaked urine. Ascending urinary tract infections usually begin in the lower parts of the urinary tract (possibly the urethra) and works its way up to the bladder and the ureters.
Skin Infections
This results from the exposure of the skin to the urine. Rashes in the perineal and anal area may cause significant discomfort to the individual.
Dehydration
This is possibly due to the frequent loss of fluids through urination
Depression
Individuals with overactive bladder may experience intense psychological problems, and this may lead to depression. Depression is usually rooted to the fact that the condition limits their physical and social capacities.
- Disturbance in the sleep cycle
- Fatigue
- Insomnia