What is Degenerative Joint Disease?
Degenerative joint disease or most commonly known as osteoarthritis is a mechanical condition involving the degeneration of the joints, which causes problems on joint movement. Osteoarthritis affects about 25 million people in the USA and is responsible for about 50% of all prescriptions for non-steroidal anti-inflammatory drugs. Osteoarthritis commonly affects people aged 65 years old and above.
Osteoarthritis was taken from the terms “osteo” (bones),” arthro” (joints) and “itis” (inflammation), which means inflammation of the bone joints. However, degenerative joint disease does not really involve the inflammation of the joints. What happens in osteoarthritis is that there is a degradation of the cartilage and synovium between the joints, which leads to the contact and friction between the two bones of the joint. Because of the absence of inflammation, degenerative joint disease is also known as osteoarthrosis. Osteoarthritis also results in atrophy of the muscles and ligaments because of decreased joint movement.
Degenerative joint disease may be primary or secondary. Primary osteoarthritis does not result from other underlying causes, while secondary osteoarthritis results from an underlying medical condition.
Osteoarthritis commonly affects the joints of the hands, spine, feet and weight bearing joints such as the knees and hips. Other joints may also be affected.

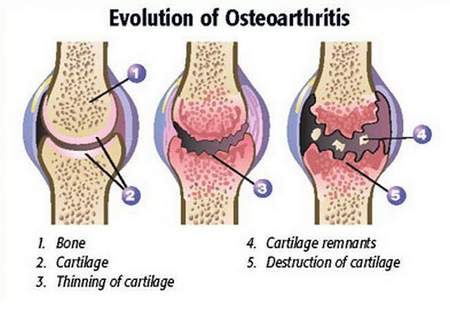
Picture 1 – Degenerative Joint Disease (osteoarthritis) of knee
Symptoms of Degenerative Joint Disease
The symptoms of osteoarthritis results from the degeneration of the cartilage in between the joints, leading to:
- Sharp pain on the joint, aggravated by cold and humid environment, usually bilateral
- Burning sensation
- Loss of joint movement
- Stiffness
- Crepitus or presence of crackling sound when the joint is moved
- Muscle spasms around the affected joint
- Joint appears larger due to collection of excess fluid on the knee joint or “water on the knees”
- Presence of Bouchard’s nodes in the proximal interphalangeal joints
- Presence of Heberden’s nodes in the distal interphalangeal joints
- Nodes may be painful and may limit the movement of the joint
- Bunions on the toes (swollen and reddish protrusion on the joint of the big toe)
Causes of Degenerative Joint Disease
The presence of osteoarthritis may be associated with certain causes and risk factors. Previous beliefs say that degenerative joint disease is caused by mechanical injury such as exercise, however, more recent studies has not found any association between osteoarthritis and exercise in normal individuals. Cracking of the knuckles and toes also do not have any association with the occurrence of osteoarthritis. Causes of degenerative joint disease include the following depending on the type of osteoarthritis:
Primary Osteoarthritis
The causes of primary osteoarthritis include:
Aging. Aging causes the fluid in the cartilage to diminish because of a reduction in proteoglycan. Proteoglycan is responsible for protecting the joint and a reduction of it can lead to joint degeneration.
Heredity. Primary osteoarthritis may also be inherited. In fact, identical twins have a high risk for developing the disease when the other twin or sibling already develops it because of certain genetic factors.
Secondary Osteoarthritis
Secondary osteoarthritis develops following certain medical conditions that destroy the joints and cartilages. These include:
Obesity. Being obese or overweight gives undue tension on the weight-bearing joint. As a result, the cartilage and synovium undergoes degeneration from the increased force between the bones. This eventually leads to wearing of the cartilage and contact of the bones with each other.
Other causes include
- Congenital joint disorders
- Injury to the joint
- Diabetes
- Other forms of arthritis that increases joint degeneration
- Instability of the ligaments
- Septic arthritis
- Marfan syndrome
- Wilson’s disease
- Hemochromatosis
Pathophysiology of Degenerative Joint Disease
Osteoarthritis involves the degeneration of the joint specifically the subchondral bones and the cartilage. The cartilage is the tough and elastic tissue found in between the bones that is responsible for joint movement. The cartilages often do not have a blood supply and it gets nutrients and oxygen through diffusion from surrounding blood vessels. The movement of the joint also is guided by the synovial fluid between the joint. Without this fluid, it becomes very difficult for the joint to perform its range of motion. The synovial fluid serves as a grease to allow smooth joint movement.
Because of aging and certain medical conditions, the cartilage and synovial fluid degenerate and disappear. As a result, the surface at the end of the bone comes in contact with the surface of the other bone, creating excessive tension and friction between the bones. This condition results in the hardening of the bones involving the joint, which causes stiffness. The constant pressure and friction between the bones also result in pain. When byproducts of joint degeneration collect in the synovial space, the body responds by initiating an inflammatory response to repair the joint injury. The synovium also compensates by producing more fluid to increase the lubrication in the joint leading to swelling of the joint. The constant friction between the bones also leads to new bone growth known as osteophytes. The lack of cartilage and the bone outgrowth further leads to pain that is usually bilateral.
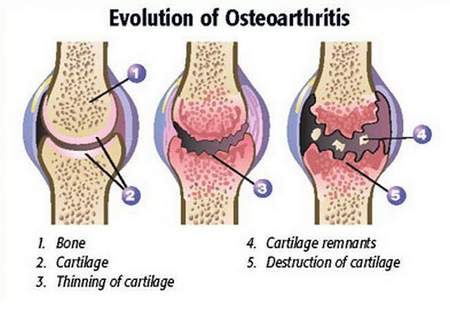
Picture 2 – Degenerative Joint Disease Pathophysiology
Diagnosis
The main diagnostic test for osteoarthritis involves imaging studies to visualize the joint. These include:
X-rays are the basic diagnostic procedure for the disease. In x-rays, the common finding is a narrowing of the joint space, increased bone formation, osteophyte growth as well as cyst growth due to increase in the synovial fluid. X-rays also differentiate osteoarthritis from other joint diseases such as rheumatoid arthritis and gouty arthritis. Radiographic studies also rule out the presence of fracture in a joint, which is similar to the symptoms of degenerative joint disease
Treatment
Treatment for degenerative bone disease involves reducing the causative factor as well as managing the signs and symptoms of osteoarthritis which include:
1. Reduction of causative factor
- Adequate exercise. An acceptable level of exercise is required for people with moderate osteoarthritis to enhance the joint mobility and reduce pain. The pain associated with osteoarthritis usually is relieved by a moderate activity. Exercises include active range of motion exercises and graded exercises. Weight lifting and weight bearing exercises involving the affected joint should be avoided to prevent further injury to the joint.
- Weight reduction. For overweight and obese patients, reducing the weight is an important management to prevent added weight on the affected joint. The reduction in the weight also reduces the need for pain medications.
2. Medications
- Analgesics. Analgesics are the primary medications for reducing pain in osteoarthritis. The most commonly used analgesic is acetaminophen. This medication may be used in mild pain associated with osteoarthritis.
- Anti-inflammatory Drugs. Moderate to severe pain in osteoarthritis may require the use of NSAIDs or non-steroidal anti-inflammatory drugs. Ibuprofen is the most prescribed medication; however it may lead to gastrointestinal irritation and bleeding with prolonged use. Because of this, COX-2 inhibitors, a newer form of NSAIDs, in the form of celecoxib may be given to reduce gastrointestinal side-effects. NSAIDs may also be administered through topical applications, but may have lesser analgesic effects.
- Opioid Analgesics. Pain that is not responsive with analgesics and NSAIDs may be managed using more potent analgesics such as morphine and fentanyl; however, their use should be monitored because these may result in adverse effects such as respiratory depression.
- Steroids. Injectable steroids may also be used as a treatment for more severe case of osteoarthritis to reduce the inflammation, pain and swelling.
- Glucosamine and Chondroitin Sulfate. These substances are available as dietary supplements. These are natural components of the joint, which is thought to increase the cartilage formation and production of synovial fluid in the joint.
- Newer Medications. New types of medications such as monoclonal antibody medications have been studied to reduce the symptoms of osteoarthritis. Tanezumab is a monoclonal antibody medication that is found to reduce pain and enhance joint function.
3. Surgery
Advanced cases of degenerative joint disease may be managed through joint replacement surgery. The most common site for joint replacement surgery involves the hips and knees because a severe degeneration of these joints leads to major difficulties in mobility.
4. Conservative Treatments
Manual therapy may also be essential in reducing pain associated with osteoarthritis. Splinting the joints such as of the hands may also hasten healing and prevent further injury.
5. Alternative Therapies
Other conservative treatments for osteoarthritis include the use of ginger, omega-3 fatty acids, Vitamins A, C and E. These substances are believed to produce anti-inflammatory effects thereby reducing pain and swelling. Acupuncture is also used for the reduction of pain and improvement of the joint function. Finally, mud pack therapy may also help in reducing the inflammation by the use of minerals found in mud pack.
Complications
Complications of degenerative joint disease include:
- Permanent loss of function
- Severe pain
- Tissue necrosis of the surrounding tissues
- Infection of the joint as a result of open wound or injury
- Joint deformities
In order to avoid osteoarthritis and prevent the occurrence of complications that may be debilitating, preventive measures should be instituted. These include weight reduction to prevent undue tension in between the bones of the joint. Maintaining an active lifestyle also helps in promoting the range of motion of joints. Other underlying conditions should also be managed to prevent degeneration of the joint as a complication.