Heparin Induced Thrombocytopenia
Definition of Heparin Induced Thrombocytopenia
Heparin-induced thrombocytopenia or HIT is defined as the clinical condition where an individual under heparin treatment suffers from thrombocytopenia. We can better understand the disease by knowing what are heparin and thrombocytopenia.
What is Heparin?
Heparin is a medication that belongs to the class of anticoagulants. Anticoagulants are agents that prevent the blood from clotting or coagulating. Blood clotting or coagulation is the process in which the blood assumes a semi-solid state (called blood clots) instead of its normal liquid state. Blood in the form of a clot may block blood vessels and affect vital organs such as the heart, lungs, and brain.
What is Thrombocytopenia?
Thrombocytopenia is the condition where an individual’s platelet count is decreased by almost 50 percent or when an individual’s platelet count is less than 100×103/L. If thrombocytopenia occurs at around 5 to 14 days following the start of heparin therapy, then it is likely to highly suspect HIT. This condition causes prolonged hospital stay and even possibly high morbidity and mortality.
What is the Mechanism behind HIT?
The mechanism behind HIT is said to be similar to how the body reacts when exposed to an allergen. Immune reaction plays a significant role in the cascade of events seen in HIT. It is a complex process, but it can be summarized in the following events:
1. Exposure to heparin triggers the immune system to recognize it as a “non-self” agent, even if heparin naturally occurs in the body.
2. The immune system then creates antibodies against heparin, especially when heparin binds to platelet factor 4.
3. The antibodies then react to the heparin bound in platelet factor 4; this reaction then causes the activation of platelets.
4. When platelets are activated, the body starts to form blood clots and platelet microparticles; this formation exhausts the body’s platelet reserve which causes the platelet count to drop significantly (i.e., thrombocytopenia).
Contributing Factors to HIT
Heparin use
A primary factor contributing to the emergence of HIT is the previous or constant use of heparin. Individuals with HIT were found to have previous exposure to heparin. A majority of patients with HIT were also found to possess the HIT antibodies while receiving doses of heparin.
Role of antibodies
The presence of the IgG antibodies is also seen as a contributing factor. IgG antibodies are the type of antibodies that are activated in cases of microbial infections. This class of antibodies is immediately developed (usually about 5 days) upon exposure to a bacteria or a chemical agent (e.g. heparin) and lasts even if the bacteria or the chemical agent is removed from the body. It is still possible for an individual to have a reaction to heparin even if the heparin treatment has been discontinued.
Symptoms of HIT
- Thrombocytopenia, i.e., a platelet count below 100×103/L or a platelet count decrease of almost 50 percent
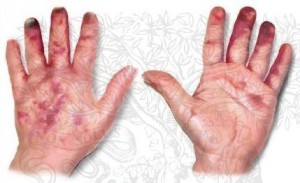
- Appearance of rashes or red spots on the skin
- Enlargement of a previously existing blood clot
- Development of new blood clot in any part of the body (mostly in the veins and arteries)
If a clot develops, the patient may have the following signs and symptoms:
- Severe leg or calf pain (which may indicate deep vein thrombosis)
- Chest pain and breathing difficulty (which may suggest a clot formation in the heart or lungs)
- Loss of consciousness, drowsiness, and changes in movement and sensation (which may indicate a clot formation in the brain)
For patients with heparin given intravenously or through the blood, the following signs and symptoms may be experienced:
- Tachycardia (abnormally fast heart rate)
- Shortness of breath or breathing difficulty
- Chest pain
- Fever and chills
- High blood pressure
Diagnostic Tests for HIT
HIT can be diagnosed by physicians by the following:
1. Clinical scoring
Physicians may follow a type of scoring when it comes to diagnosing HIT. The clinical scoring for HIT involves 4 Ts which stand for:
- Timing
- Thrombocytopenia
- Thrombosis
- The absence of any other explanations
The patient is assessed for symptoms, and a corresponding score is given; if the patient’s scores 6-8 on the scale, then there is a high probability that the patient has HIT.
2. Platelet monitoring
Another way to confirm if the patient, indeed, has HIT is to monitor the platelet count. Those receiving heparin treatment are usually monitored for their platelets on a daily basis.
3. HIT antigen and antibody activation assays
These two laboratory tests are done to detect the presence of HIT antibodies in the patient’s blood. These tests usually target PF4, the protein with which heparin binds. Results from these two laboratory tests would confirm the presence of HIT.
Treatment Guidelines for HIT
Once the individual manifests signs of HIT, treatment guidelines are immediately implemented. Treatment usually involves the following:
1. Discontinuing and avoiding heparin in any form (whether that is a heparin flush or a heparin catheter) and route.
2. Providing direct thrombin inhibitors. These are medications which delay the process of blood clotting to prevent the exhaustion of the platelet reserves in the body. Examples of direct thrombin inhibitors are:
- Argratroban
- Lepirudin
- Desirudin
- Bivalirudin
- Ximelagatran
3. Confirming the presence of HIT antibodies by letting the patient test for Anti PF4 test
4. Avoiding platelet transfusion
5. Facilitating platelet recovery
6. Assessing and monitoring the patient for deep vein thrombosis or clot formation in the lower extremities