Reactive Airway Disease in Children, Adults – Symptoms and Treatment
What is Reactive Airway Disease?
Reactive Airway Disease is a condition involving the antigen-antibody reaction in the lung and the activation of the inflammatory cascade that results in airway inflammation. Reactive airway disease should not be confused with asthma, as the disease is broader than asthma in children and adults. Patients may experience wheezing without asthma. However, the manifestations and management of reactive airway disease and asthma is synonymous.
Reactive airways disease affects up to one-third of the population in children. Reactive airway disease accounts for up to 200,000 hospitalizations and 13 million healthcare visits in the United States. Reactive airway disease is common in Hispanic and black children. In fact, hospitalizations from reactive airway disease is four times higher in African Americans that in whites. Reactive airway disease also affects both children and adults with the peak of affectation in children during the ages six to eleven.
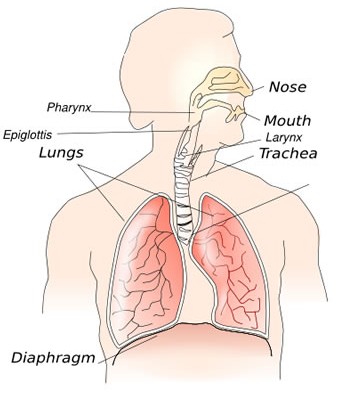
The mechanism of the disease involves narrowing of the airways as a result of bronchoconstriction and airway inflammation with resulting production of lung secretions. The changes in the airways results from the activation of an inflammatory response and immunity because of an antigen inhaled into the lungs.
Symptoms of Reactive Airway Disease
Reactive airway disease symptoms result from the inflammatory cascade that happens in the lungs. Asthma may also be a sign of reactive airway disease, making the two interchangeable.
Symptoms of reactive airway disease include:
- Fever – Fever may be a sign of ongoing infections and the inflammatory process in the lungs as a result of an antigen-antibody reaction.
- Dyspnea and Tachypnea – because of airway affectation, patients also exhibit fast breathing because only a small percentage of oxygen is enhaled. Dyspnea is experienced because of significant narrowing of the bronchioles.
- Wheezing – Wheezing is a high-pitched sound heard during expiration as a result of the airway narrowing.
- Coughing – The patient may also exhibit coughing as the lung’s way of eliminating the allergen or secretions.
- Tachycardia – Patients may also experience fast heart rate because of the body’s attempt to deliver more oxygen to the cells.
- Flushing and cyanosis – A flushed face or body is an early sign of hypoxia because the body compensates to increase oxygenation by increasing the blood flow. However, the blood may only carry small amounts of oxygen due to respiratory compromise. Prolonged hypoxia may eventually lead to cyanosis.
- Nasal Flaring – Nasal flaring is a sign of respiratory distress as they body attempts to increase oxygen inhaled through the nose.
- Intercostal retractions – There will also be retractions of the intercostal muscles because of severe respiratory compromise.
- Hyperresonance of the lungs – Hyperresonance may indicate lung consolidation because of accumulation of pulmonary secretions.
- Altered mental status -Poor oxygenation may also affect the brain cells and lead to altered levels of consciousness.
- Allergic shiner – These are dark semicircles under the eyes as a result of allergic reactions.
- Barrel chest – Patients may also exhibit an increased anteroposterior diameter of the chest because of severe lung consolidation.
- Clubbing – Persistent hypoxia of the peripheral areas of the body leads to clubbing of the fingers.
Causes of reactive airway disease
Causes of reactive airway disease are synonymous with asthma. Causes of reactive airway disease include:
- Environmental Factors – Substances such as molds, tobacco smoke, pollen, pet dander, exercise, stress and weather changes can cause irritation of the airways and may lead to reactive airway disease.
- Respiratory infection – Infections with respiratory syncytial virus and Mycoplasma pneumonia are also found to cause antigen-antibody reaction in the airways.
- Mediastinal mass – A tumor or any mass in the mediastinum can cause compression of the airway, leading to difficulty breathing.
- Tracheoesophageal fistula – Tracheoesophageal fistula is a small connection between the trachea and the esophagus. As a result, food particles from the esophagus can get inside the trachea and cause allergic reactions from the substance and cause respiratory distress to individuals.
Treatment for reactive airway disease
The treatment for reactive airway disease involves medical managements to control the symptoms such as:
Medications. Respiratory medications are the first line of treatment for reactive airway disease to improve lung capacity and dilate the airways. Medications may involve:
- Beta adrenergics – Beta adrenergic drugs are given to relax muscles in the airways that further lead to bronchodilation. When the bronchioles are dilated, there is more oxygen that goes into the lungs and eases breathing. Beta adrenergics are commonly given via inhalation or nebulization.
- Theophylline – Theophylline is also a bronchodilator that helps dilate the airways. Theophylline is commonly given via the intravenous route.
- Corticosteroids – Corticosteroids such as prednisone or budesonide may also be given via the intravenous or inhalation route. Corticosteroids are potent anti-inflammatory drugs that limit the chemical mediators in order to relive airway inflammation. This drug also limits the production of pulmonary secretions.
- Mucolytic and expectorants – These cough remedies are usually given to aid the expectoration of secretions from the lungs. Children and adults with altered mental status may need airway suctioning in order to effectively clear the airways.
- Antibiotic therapy – Patients suffering from secondary bacterial infection of the lungs may also require antibiotic treatment in the form of broad spectrum antibiotics.
- Oxygen therapy – Patients with problems in oxygenation may also receive oxygen therapy via a nasal cannula or face mask.
Reactive Airway Disease in Children
Reactive airway disease in children may come in the form of asthma. Children are often affected with asthma because of hypersensitivity to environmental factors such as dander and weather changes. Children often outgrow reactive airway disease, but some may have persistent condition during adulthood.
Reactive Airway Disease in Adults
Adults may also experience reactive airway disease but have lesser incidence than children due to the fact that the immune system has already adapted to the causative factors such as allergens. However, the presence of reactive airway disease that has persisted from childhood may cause severe lung problems such as chronic obstructive pulmonary disease and emphysema or the lack of elastic recoil of the alveoli due to chronic lung consolidation.