Prolapsed Uterus – Pictures, Symptoms, Surgery, Treatment
What is Prolapsed Uterus?
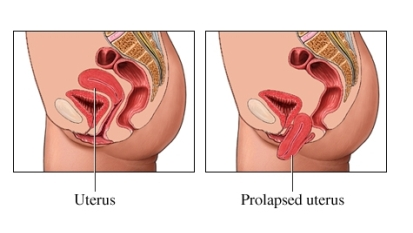
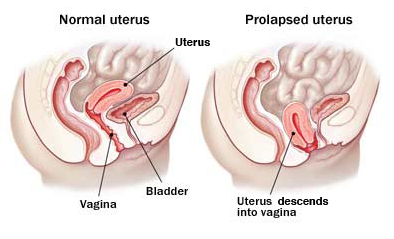
The uterus is a pear shaped, hollow, muscular organ of tghe female reproductive system. It is about 7.6 cm or 3 inches long and in which the fetus develops during pregnancy; the other term used for uterus is womb. The fertilized ovum enters the uterus where implantation happens. The uterus also gives nourishment to the growing fetus from blood vessels. It is located inside the pelvic cavity, near the urinary bladder and upwards toward the rectum.
A prolpased uterus is a condition in which the uterus falls out into the vagina from its original location. Most of the time, a prolapsed uterus is accompanied by a cystocele (Prolapsed Bladder) and/or Rectocele (anterior displacement of the rectum into the vagina).
The extent of the prolapse varies; it can be a slight sagging of the uterus, but in more complex cases, it can be a complete downward displacement of the uterus to the vagina. It can be classified as the following:
First degree
The cervix can be seen when labia is spread without straining or traction.
Second degree
The cervix protrudes out to the level of the perineum.
Third degree
Most of the uterus or the entire part of it protrudes out of the vagina and into the perineum.
Studies shows that 50% of all women who have symptoms of uterine prolapse are those above 50 years of age due to weakening and less elasticity of the pelvic muscles. It is more common among Hispanic women. Next are Asians and blacks.
The other names of a prolapsed uterus are uterine prolapse, pelvic relaxation, or pelvic relaxation.

Image Source: www.2womenshealth.com
Pathophysiology
The uterus placed inside the pelvic cavity, near the bladder and towards to the rectum. It is divided into four sections: the fundus, internal OS, corpus, and the cervix.
It is supported by muscles and ligaments. Uterine prolapse happens if this supporting structure is weakened. The uterus may slip down the vaginal canal and even extend outside the vaginal orifice. When the uterus falls down, it may also pull the other nearby organs like vaginal walls, bladder, and rectum.
Signs and Symptoms
- Lower back pain
- Abdominal pain
- Presence of tissue protrusion from the vagina
- Heaviness on the Pelvic area
- Vaginal Discharge
- Constipation
- Fecal incontinence
- Urinary incontinence
- Urinary retention
- Painful sexual intercourse or Dyspareunia
- Protrusion of the cervix during examination
Causes and risk factors
Vaginal childbirth
Damage to the muscles supporting the uterus is likely because of compression and increased pressure from the fetal head and maternal forces during delivery. It causes stretching and tearing in the muscles. Obstetric trauma to the muscles also occur during vaginal delivery.
Multiple pregnancy
Uterine prolapse is more common among women with more children.
In addition to this, other risk factors include:
- Increased age
- Menopausal period
- Because of a decrease in estrogen after menopause, the muscle loses its strength and is weakened.
Obesity
Due to increased strain on the muscles that support the uterus.
- Chronic constipation
- Smoking
- Prolong standing
- Heavy lifting – because of intra-abdominal pressure
- Other diseases like COPD and chronic cough.
Diagnosis
Complete pelvic examination
The doctor will conduct a pelvic examination to look for a protruding uterus. This is done while lying down and standing up. To assess for the degree of the prolapse, you will be asked to bear down like you’re doing bowel movement.
Pelvic ultrasound
This is done to further assess the degree of the prolapse.
Magnetic resonance imaging (MRI)
It is not commonly done but can be an option in determining the stage of prolapse.
Treatment
Treatment depends on the degree of the prolapse. For a mild prolapse, usually no treatment is needed. For more severe degrees or symptoms, there are available treatments both non-surgical and surgical.
Pessary
A vaginal pessary is inserted into the vagina to support the uterus and prevent it from falling down. Minimal discomfort and irritation can be felt since it presses the vaginal muscle. Prolonged usage of pessary may lead to necrosis and ulceration. Pessary should be cleaned frequently and removed every one to two months.
Surgery treatment includes:
Total Hysterectomy
The complete removal of the uterus is performed for severe degrees of uterine prolapse.
Vaginal Hysterectomy
A surgical procedure used to correct sagging of the supporting muscle of the pelvis. Ligament are preserved so they may continue their functions as support of the pelvic muscle and help improve muscle tone.
Sacrospinous fixation
This operation involves attaching the vaginal vault to firmer tissue and muscle within the pelvis to lift it back into place. It is done through the vagina, so there is no need to make an incision (wound) on the abdomen. Two non-dissolvable stitches are sewn into the sacrospinous (pelvic) ligaments and muscle which are then passed through the top of the vagina. The stitches are tightened against the muscle so the vagina is pulled back into place. Dissolvable stitches are then used to close the vaginal wall.
Kegels Exercise
This exercise strengthens the pubococcygeus muscle of the pelvis. To do this, women will sit on a toilet and she will contract the pelvic muscle for few seconds and relax slowly after. It is suggested that patients practice this when they have a full bladder and repeat the exercise for at least ten minutes.
Estrogen Replacement
During menopause, women will lose estrogen that helps strengthen the pelvic muscle. Taking estrogen replacement may help maintain muscle tone and prevent weakness that may lead to uterine prolapse.
Complications
Uterine prolapse, if left untreated, will progress to more complicated cases like other Pelvic Organ prolapse. Cystocele, or prolapsed bladder, and Rectocele, a prolapsed rectum, are known complication of uterine prolapsed.
Urinary tract infection, ulcers, and constipation may also occur in severe cases of pelvic organ prolapse.
Prevention
To decrease the possibility of having uterine prolapse, practice the following preventive measures:
- Maintain your ideal weight
- Do kegels exercise
- Maintain daily movement to prevent constipation
- Stop smoking
Prolapsed Uterus Pictures