Pain in Heel of Foot
Pain experienced in the heel of the foot is one of the most common pains experienced by people. This pain can cause severe discomfort and can affect one’s ability to work or complete day-to-day tasks.
Introduction to Pain in the Heel of the Foot
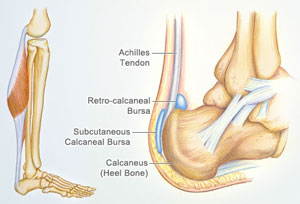
When a person moves, walks or stands, the calcaneus or the heel bone distributes the compressive forces caused by these activities. This part of the foot receives the most stress. The force applied in the heel can cause injuries, and the injuries then causes heel pain. Several injuries and conditions may cause heel pain.
What Causes Pain in the Heel of the Foot?
As said earlier, there are several causes for that pain felt in the heel of the foot.
1. Plantar Fasciitis
This is a condition where there is inflammation on the connective tissue found on the sole or the bottom of the feet. The connective tissue is called plantar fascia, the stretch of the tissue is from the sole of the foot to the toes. This is considered a common condition that afflicts an average of 2 million Americans per year. The condition is often a result of overuse of the plantar fascia (the connective tissue) or the arch tendon in the foot, from weight-bearing activities. The condition is also seen among obese individuals and athletes, especially runners.
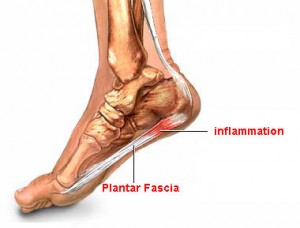
Plantar Fasciitis
Individuals may experience plantar fasciitis under the following circumstances:
- Individuals with flat foot
- If the foot has a high arch
- Excessive pronation of the foot or a foot that is positioned inward when walking
- Standing or running for long periods of time on hard surfaces
- Overweight individuals
- Wearing shoes that are worn out or those that don’t fit well
- Tight calf muscles or Achilles tendon
Symptoms of Plantar FasciitisHeel pain is one of the symptoms of the condition, but other symptoms associated with the condition can also be experienced. The symptoms include:
- Stabbing pain felt in the foot
- Pain upon taking the first steps after getting out of bed
- Pain felt after sitting for a long period of time
- Pain that gets worse as the day goes on
- Difficulty walking or moving
- Difficulty of bending the foot towards the shin
- Knee pain
2. Achilles Tendinitis
Another possible condition that can cause heel pain is Achilles tendinitis. This is the inflammation of the Achilles tendon, the tendon connecting the calf muscles to the heel bone. People engaging in high impact activities such as jogging, tennis, or racquetball are at risk for this injury. Individuals born with a short Achilles tendon are also at risk for this condition.
Achillies Tendinitis
Symptoms of Achilles Tendinitis
- Heel pain upon walking and running
- Pain or stiffness felt during the morning
- Tender Achilles tendon
- Swollen or warm skin surrounding the Achilles tendon
- Difficulties standing up
3. Bursitis
Heel pain can also be a result of bursitis. Bursitis is the inflammation of a fluid filled sack called, bursa. Bursa can be found beneath the heel.
Achilles Bursitis
Symptoms of Bursitis
- Heel pain especially when running or walking
- Pain that gets worse when standing on tiptoes
- Inflammation of the skin surrounding the heel bone
4. Haglund’s Deformity
This deformity is characterized by a bony growth that surrounds a tender tissue at the back of the heel. It usually results from repeated rubbing of the back of the heel against the shoes. It often occurs in women wearing high heels but the condition may also develop among runners.

Haglund’s Deformity
Symptoms of Haglund’s Deformity
- Heel pain
- Swelling and a noticeable bump located at the back of the heel
- Inflammation and redness in the heel area
Treatment for Pain in Heel of the Foot
Treatment depends on the underlying condition associated with the pain. But generally, the following treatment approaches are done to relieve heel pain.
1. Reduction of Inflammation
Heel pain is often accompanied by inflammation. Inflammation is treated with the use of corticosteroids and Non-Steroidal Anti Inflammatories. Corticosteroids effectively reduce the inflammation; these medications may be given orally or through injections. In some cases where severe inflammation is experienced, corticosteroids are administered through an electric current in a process called iontophoresis.
Non-steroidal Anti Inflammtories or NSAIDs are also given, these aid in reducing the inflammation and relieving the associated pain. NSAIDs can are given orally and can be acquired over the counter; examples of NSAIDs are ibuprofen and aspirin.
2. Stretching and Other Exercises
Exercise and stretching aids in strengthening the injured tendons and connective tissues, when these are strengthened, injuries are reduced and therefore pain is avoided. Gentle stretching of the injured foot, raising the heel and putting the hands against the wall and leaning on them are just some of the exercises that may strengthen the tendons and connective tissues.
3. Use of Sturdy Shoes and Insoles
Wearing sturdy shoes with thick soles and rubber heels can also treat heel pain. Shoes with these features relieve pressure and provide ample support to the foot.
4. Splints
Splints are devices that help immobilize a specific part of the body. There are evidences that suggest the use of splints may help relieve pain and facilitate the healing of the injured heel. L shaped splints secured by Ace bandages can help stretch the leg while sleeping; the stretching allows the tendons to heal and also prevents strictures and pain felt during the morning.
5. Orthotics
For severe cases of heel pain, the use of orthoses might be prescribed. Orthoses are devices applied to a body part to correct or modify its structure. Braces and other corrective devices are examples of orthoses and are used to restrict movement, control and guide a joint or an extremity. The use or orthoses are usually indicated for patients with deformities such as a flat foot, short Achilles tendon and high arches. The deformities cause imbalances and puts strain on the structures surrounding the heel of the foot.