Heel Pain – Causes, Treatment, Relief, Types, Diagnosis
What is Heel Pain?
Heel pain is a condition in which weight-bearing on the heel causes discomfort. It i a common foot problem where pain usually occurs underneath or behind the heel where the Achilles tendon attaches to the bone.
Types of Heel Pain
a. Achilles Tendinitis
- An inflammation of the tendon that connects calf muscles to the heel bones.
- Overuse of Achilles tendon can cause inflammation, pain, and swelling.
- It is caused by overuse of the affected limb and this condition is most common in people who engage in exercises like jogging, running or who play tennis.
- The Achilles tendon is considered the largest tendon in the body which primarily used for running, walking and jumping.
- The Achilles tendon doesn’t have good blood supply, so when injury occurs, it heals slowly.
- Cause: It is more likely to occur after an increase in intensity or amount of activity such as playing basketball and (b) when the calf muscles are not stretched.
- Symptoms: (a) pain in the back of the heel which usually worsens with activity (b) pain and stiffness along the Achilles tendon in the morning (c) severe pain the day after exercising (d) thickening of the tendon as a result of swelling (e) painful when touched or moved (g) swollen and warm to touch (f) tenderness, especially during palpation
- Diagnosis: (a) history of prior injuries (b) physical examination: (1)the doctor will palpate the location of the injury and look for signs of tenderness, swelling, and pain in the area of tendon when you stand in your toes. (2) The doctor will also check for passive and active range of motions and reflexes of the knees, ankle and feet. (c) Imaging test like X-rays can show if the tendon have become calcified or hardened, and magnetic resonance imaging (MRI) can help look for tears within the tendon.
- Treatment: (a) cold compress (b) wearing heel pads to reduce stress in the tendon (c) an exercise routine to help strengthen the tendon (d) rest to prevent the situation becoming worse
- (e) NSAIDS or non-steroidal anti-inflammatory drugs like ibuprofen to reduce inflammation and pain (f) manual therapy that treats musculoskeletal pain or injury comprised of massage therapy, and joint mobilization and manipulation. (g) If these treatments do not improve symptoms, surgery is recommended to remove bone spur that irritate the tendon. (h) Extracorporeal shock wave therapy that uses low dose of sound waves to stimulate the healing process in the damaged area. It is not an invasive procedure, so it is recommended before surgery, but it doesn’t have a consistent result.
b. Bursitis of the heel
- It is also called Retrocalcaneal bursitis
- Is an inflammation of the bursa, a small sack of fluid beneath the heel bone.
- A bursal sac is filled with slippery fluids that acts to lubricate and helps reduce friction between the muscles and the tendons. It acts as a cushion or shock absorber between tendons and the bone.
- It is located between the Achilles tendon and the heel bone.
- Cause: (a) when a person increases their level of physical activity like too much walking and running, it irritates and inflames the bursa (b) over-using ankles by doing repetitive actions (c) ill-fitting shoes (d) or medical problems like rheumatoid and gouty arthritis.
- Symptoms: (a) pain in the heel especially when running or walking, and even when the area is touched (b) extreme pain especially when standing on tiptoes (c) tender feel when it is palpated (d) warm to the touch and redness the skin over the back of the heel.
- Diagnosis: (a) prior injury history (b) physical examination that involves checking the infected part for pain, redness, swelling, and warmth (c) imaging tests like X-rays which can show if the tendon has become calcified or hardened, and magnetic resonance imaging (MRI) which can help evaluate a patient for tears within the tendon.
- Treatment: (a) manual therapy treats musculoskeletal pain or injury and is comprise of massage therapy, joint mobilization and manipulation (b) activity modification: avoid activities that cause pain (c) cold compress (d) exercise that will improve strength, flexibility and balance (e) NSAIDS or non-steroidal anti-inflammatory drugs like ibuprofen to reduce inflammation and pain (f) ultrasound treatments help reduce the inflammation (g) normally this type of disease doesn’t require surgery
c. Excessive Pronation
- Pronation is a normal adaption of the foot to adapt on uneven surfaces while walking and it also helps absorb shock.
- Excessive pronation is where the foot turns inward and soft tissue stretches and causes stress and inflammation on the planter fascia ligament.
- Cause: (a) very common for flat-footed persons (b) trauma from sports or repeated stress from wearing high-heeled shoes for long periods of time (c) shoes lacking adequate support through the arch
- Symptoms: (a) Achilles tendinitis (b) bunion (c) heel spurs (d) plantar fasciitis (e) ankle sprain (f) knee, hip, lower back pain (g) corns and calluses (h) hammertoes or contracted toes which is a result of wearing ill-fitting shoes; the toes became bent like a hammer (i) shin splints or lower leg pain
- Diagnosis: (a) history of prior injury (b) physical examination checking the infected part for pain, redness, swelling, and warmth of the heel area (c) there is a test to detect excessive pronation: (1) the Achilles tendon test where the person will stand in front of the mirror and look at the back of the legs and foot. On a normal foot, the tendon and the heel run straight down, but in excessive pronation, the tendon runs straight down the leg but twist outwards at the heel. (2) A “used shoes” test where you look at your used running shoes with the toes pointed away from you; if your shoes tilt inward, it shows that your feet are excessively pronated.
- Treatment: (a) anti-pronation insoles provide a supprt system that helps aligns the lower body (b) wearing supportive shoes that give ample support and cushioning particularly at the heel and arch of the foot (c) surgery is not that reccomended in this type of heel problem
d. Haglund’s Deformity
- Known medically as posterior calcaneal exotosis that is a bony enlargement surrounded by tender tissue on the back of the heel of the bone.
- The soft tissue near the Achilles tendon becomes irritated, especially when it rubs against the shoes.
- It commonly called “pump bump” because of the high-heeled shoes that women usually wear.
- Cause: (a) high-heeled shoes or any shoes with a rigid back can cause irritation (b) heredity also plays a role in this disease (1) a high-arched foot means the heel of the bone is tilted backward into Achilles tendon and this causes the upper portion of the heel to rub against the tendon (2) a tight Achilles tendon can cause pain by compressing the bursa and a tendency to walk outside the heel that produces wear on the outer edge of the sole of the shoes that causes the heel to rotate inward.
- Symptoms: (a) a noticeable bump on the back of the heel (b) pain in the area where the Achilles tendon is attached (c) swelling, redness and tenderness on the back of the heel
- Diagnosis: (a) history of prior injury (b) physical examination checking for pain, redness, swelling, and warmth of the heel area (c) imaging tests like X-rays which evaluate the structure of the heel bone, size of the deformity and the involvement of the Achilles tendon
- Treatment: (a) ice compression (b) change of footwear (c) use of Achilles heel pads that may help reduce irritation when walking (d) NSAIDS or non-steroidal anti-inflammatory drugs like ibuprofen to reduce inflammation and pain (e) stretching exercises that will help the Achilles tendon reduce tension (f) immobilization if necessary (g) surgery is considered in severe cases to remove or reduce the bony growth
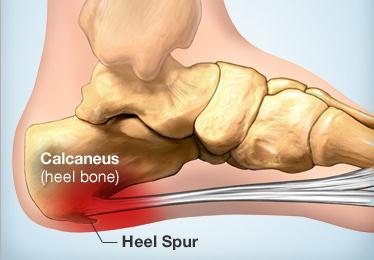
e. Plantar Fasciitis and Heel Spur Syndrome
- The plantar fascia works like a rubberband between the heel and the ball of the foot to form and support the foot’s arch. This is also a shock absorber for the body.
- It is a painful condition often caused by overuse of the plantar fascia.
- Heel spurs are a pointed bony fragment that stems from the bone and when the plantar fascia is overused, it will form calcium deposits under the heel bone as a result of inflammation. Heel spurs don’t causes pain but they are indicators that the person may suffer from Plantar fasciitis.
- Cause: (a) a common cause is very tight calf muscles that result in over-pronating that causes additional stretching of the plantar fascia (b) heredity is also included by having a high or low-arched foot (c) you walk or run on hard surfaces without enough support (d) being overweight will put strain on your heel (e) shoes that don’t fit well or are worn out (f) long-distance running
- Symptoms: (a) pain at the bottom of the foot near the heel (b) pain after exercising or any strenuous activity (c) pain is worse when you take the first step in the morning or after a long period of rest (d) sudden stretching of the foot may make the pain worse (e) after standing or sitting
- Diagnosis: (a) history of prior injury (b) physical examination checking for pain, redness, swelling, and warmth of the heel area (c) imaging tests like X-rays or an ultrasound that shows thickening or swelling of the fascia
- Treatment: (a) rest (b) massage therapy (c) stretching (d) weight loss (e) motion control shoes or shoes with thick insoles and shoes that have extra cushioning (f) warm and cold therapy (g) NSAIDS or non-steroidal anti-inflammatory drugs like ibuprofen to reduce inflammation and pain (h) stretching exercises to relieve pain (i) using extracorporeal shock wave therapy that uses low dose of sound waves to stimulate the healing process; it is not an invasive procedure so it is recommended before surgery, but it doesn’t have a consistent result (j) surgery is considered if the pain is not eased for 12 months despite other treatments