Erysipelas – Pictures, Treatment, Diagnosis, Treatment
What is Erysipelas?
Erysipelas is a Greek term that describes reddening of the skin. It is otherwise known as holy fire because of the appearance of skin. It is also termed Saint Anthony’s fire, getting its name from monks who profitably treated the disease. Erysipelas is a superficial infection of the integumentary system, specifically the skin, and caused by streptococcus bacteria. It usually affects the epidermis and extends to the lymphatics. Erysipelas has been present since the Middle Ages and caused the death of several well-known individuals, including Pope Gregory XVI.

Erysipelas Symptoms and Signs
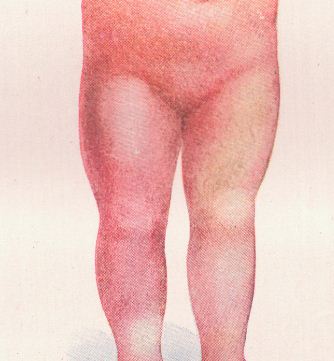
People with erysipelas commonly manifest signs and symptoms such as chills, fever, vomiting, headache, and shaking within two days of infection. Before skin lesions appear, burning and pruritus is common. Skin lesions arise and are characterized as red, warm, swollen, painful and hardened with raised edge or border. The consistency of the lesion or rash is likened to an orange peel.
Severe infections result in blisters, bullae, vesicles, petechiae, and necrosis on the skin. The rash spreads and enlarges rapidly in a few hours. It develops on the arms, face, legs, toes and fingers, but the most common site nowadays is the lower legs, accounting for almost 60% of the cases, as well as developing in fatty areas because the microorganism dwells more on these sites. Lymph node swelling may also occur as a result of systemic infection. As opposed to cellulitis, erysipelas does not produce pus. Pus is only seen in complicated and severe lesions. Serous fluids are collected under the lesion and may lead to subcutaneous edema.
Erysipelas Causes and Risk Factors
Causes of Erysipelas
Streptococcus
The most common causative microorganisms are group A beta-hemolytic streptococcus or Streptococcus pyogenes. Other species include non group A streptococcus. These microorganisms produce an exotoxin that leads to rash or lesion on non-infected sites. Streptococci are usually present in the nasal passages and cause illness after spreading to the skin.
Any skin openings
The streptococcus bacteria enter the skin through wounds, abrasions, or any minor trauma.
Risk Factors for Erysipelas
Common risk factors for the disease are:
Extremes of ages
Infants, children, and the elderly are more predisposed to develop the infection because of a compromised immune system.
Co morbidity or any underlying disease
Presence of diabetes mellitus, fungal infections, skin ulcerations, and infections increase the risk of developing erysipelas because of poor wound healing and entrance of streptococcus bacteria.
Impaired lymphatic drainage
Cases such as pelvic surgery, mastectomy, and grafting impair lymphatic circulation thus increasing the risk of developing infections.
Immune deficiency states
Decreased immune systems in cases of steroid therapy, malignancy, chemotherapy and other diseases predispose a person to acquire an infection such as erysipelas.

Erysipelas Diagnosis
Diagnosis of the disease and differentiating it from other skin infections relies on the appearance of the rash, well-demarcated and raised. An antistreptolysin O titer may be determined through blood tests after eight to ten days of infection to determine infection by a streptococcus.
Erysipelas Treatment
General symptoms of the disease generally disappear in three days while skin abnormalities usually return to normal in several weeks. Treatment of the infection involves administration of antibiotics and supportive management.
Prompt medical consultation
Erysipelas is a serious skin infection because it causes several complications involving major organs such as the heart and kidneys. Erysipelas do not heal on their own as compared to other self-limiting diseases, hence it requires prompt diagnosis and effective medical treatment.
Antibiotic therapy
Oral and intravenous antibiotics are administered to patients to destroy the bacteria. The most common antibiotic class used is penicillin and is administered for one to three weeks. Patients allergic to penicillin may be given alternative medication such as cephalosporins and macrolides. Mild forms involve administration orally but more advanced cases require intravenous antibiotic treatments. Infection from staphylococcus aureus should also be considered, hence a penicillinase-resistant antibiotic should also be used. Hospitalization for these cases is required for continuous monitoring and IV medications. To prevent recurrence of the infection, prophylactic antibiotics are also given.
Wound Care
Prevention of re-infection and complications include proper wound care. Use antiseptic solutions and creams to properly clean the area.
Dressing application
Dressings may be applied as long as it is changed every day to prevent further infection. Wet dressings are considered for necrotic lesions and should be changed two to three times a day.
Debridement
Patients who develop gangrene and necrosis may need debridement to allow faster tissue healing. Debridement involves the removal of dead skin or tissues to make way for newer ones.
Elevation of the extremities
Swelling and edema is greatly reduced by elevating the affected extremity to enhance venous and lymphatic flow. Elevate the body part with two to three pillows so as not to compromise arterial blood flow.
Use of compression stockings
These devices improve venous blood return and reduce swelling, especially in patients with impaired lymphatic drainage.
Erysipelas Prognosis
There is an excellent prognosis of the disease and takes about several weeks to heal and disappear. The infection is well-treated by the use of antibiotics. Deaths which occurred during early times were a result of an absence of specific treatment for the infection and advanced complications. Today, large spectrum antibiotics are present to effectively eradicate the bacteria.
Erysipelas Complications
Streptococcus bacteria may spread to other organs and give rise to the following complications:
Abscess and gangrene
Further tissue damage on the lesion may lead to pus formation and even death of the tissue.
Glomerulonephritis
Group A beta hemolytic streptococcus commonly infects the kidneys and produces inflammation on the glomerulus, leading to a decrease in urine output and water retention.
Thrombophlebitis
Serous fluid that collects under the skin may lead to thrombus formation and inflammation of the veins.
Endocarditis
As with glumorulonephritis, streptococci also travel to the heart and infect the endocardium (the inner muscle layer of the heart).
Toxic Shock Syndrome and Sepsis
Advanced infection allows the microorganism to replicate in the blood stream and subsequently impairs the blood vessels, leading to hypotension.
Joint and Bone diseases
Arthritis and bursitis may occur as a result of joint infection and synovial fluids.
Reoccurrence of the infection
Ten to twenty percent of patients experience re-occurrence of infection even after antibiotic therapy.
Lymphatic infection
Microorganisms and debris drains into the lymphatic system where it can proliferate again.
Necrotizing fasciitis
It is otherwise known as the “flesh-eating disease” because it involves a deeper layer of tissues. Almost 80% of patients experiencing this complication have poor prognoses.
Erysipelas Prevention
Prevention of erysipelas involves prevention of wound infection and prompt treatment of any open wounds. Good personal hygiene is also essential to prevent harboring of microorganisms such as streptococcus. Increasing immunity such as increasing vitamin and mineral intake and a balanced diet with appropriate exercise is also helpful in preventative care. The most important prevention is to avoid skin breakage because it is the primary portal of entry for streptococcus. Care for the skin by hydrating and protecting it from bio-mechanical trauma.
Erysipelas Pictures